Science
Introduction – PR1P
The Orpheus Solution
To redress the risk of blindness in premature neonates, Orpheus proposes the use of a novel peptide therapeutic, PR1P, which can be administered prophylactically to prevent ROP development long before the damaging pathologies of ROP take place.
- Prominin-1 peptide (PR1P) is a short peptide therapeutic composed of 12 amino acids that is derived from a stem cell protein known as Prominin-1 or CD133. Among the many roles attributed to prominin-1 is binding to VEGF, which potentiates its blood vessel growth-promoting (i.e., angiogenic) activity. PR1P retains this activity, binds to VEGF, and increases the response of tissues to VEGF. PR1P also stabilizes VEGF, preventing its degradation by protein-cleaving enzymes called proteases (e.g., neutrophil elastase). Through this activity, PR1P increases both the availability and activity of normal tissue VEGF. Resultantly, PR1P can promote the development of healthy, physiological blood vessel networks.
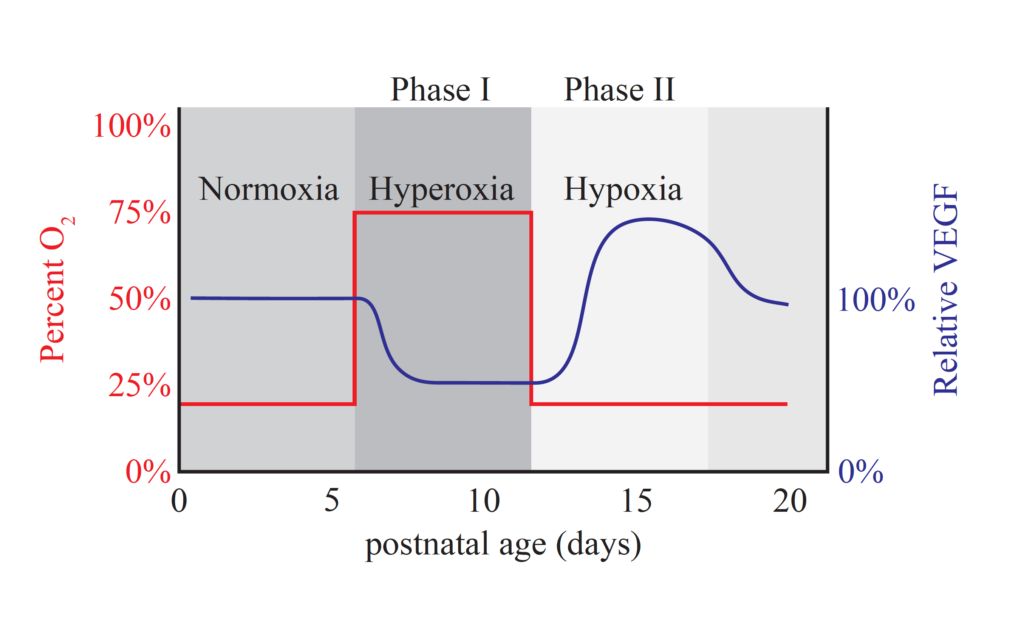
- Studies in the mouse oxygen-induced retinopathy (OIR) model—a replica of ROP in humans—indicate that PR1P prevents the development of retinopathy by preserving endogenous VEGF. In the OIR model, newborn mice are exposed to elevated oxygen levels (75% oxygen), which mimics the effects of oxygen supplementation (Figure 1). At this point, the mice enter phase I of OIR, characterized by (1) a spike in retinal oxygen, (2) declining retinal VEGF, and (3) causing the retinal vasculature to regress. After being exposed to elevated oxygen for seven days, mice are returned to normal air (21% oxygen), initiating phase II of OIR. The equivalent process in humans would occur during the transition to less invasive respiratory support with a reduction in supplemental oxygen. In this phase, VEGF levels surge, driving the development of highly disorganized blood vessel networks in the retina (i.e., pathological neovascularization).
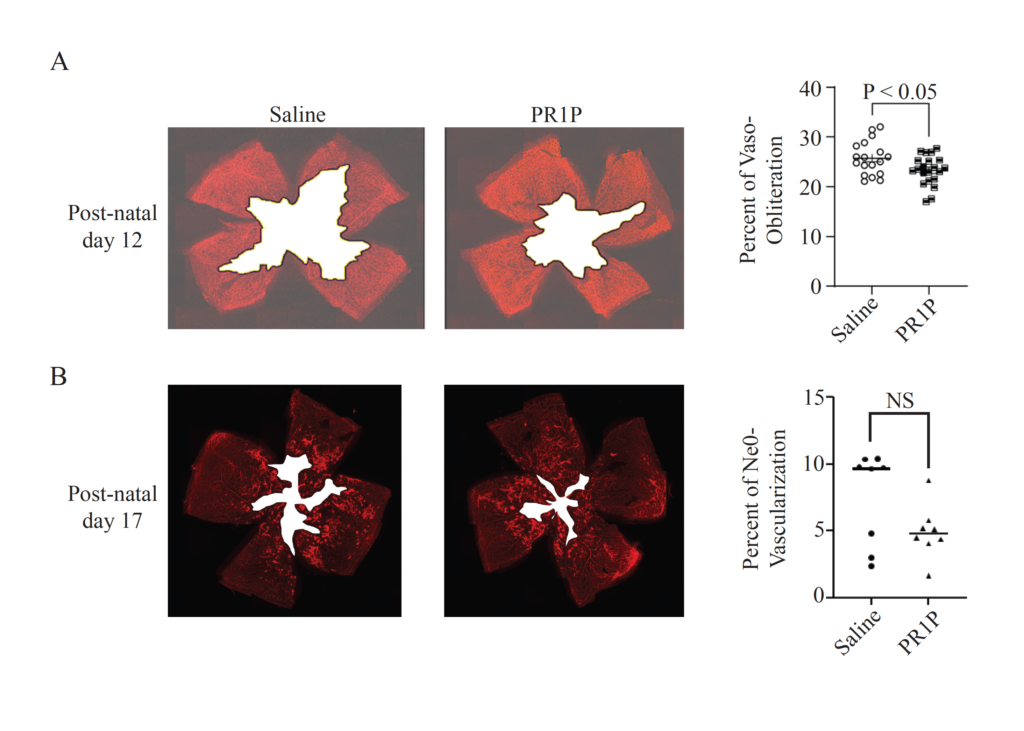
When newborn mice are given injections of PR1P, VEGF levels are retained during phase I, preventing the stalling and regression of retinal vascular development (Figure 2). In essence, the retinal vasculature develops normally, as would occur without oxygen supplementation in mice—or in utero in humans. When these animals are returned to normal levels of oxygen, the appropriately developed retinal vascular bed provides sufficient oxygen to the tissue, preventing the surge in VEGF and subsequent pathological neovascularization. Translated to human babies, these results imply that PR1P can prevent early-stage and late-stage ROP when administered alongside respiratory support with oxygen supplementation.
Retinopathy of prematurity (ROP)
The development of the retinal layers and its vasculature begins around 16 weeks of gestation; however, completion of this vascularization process only occurs at full term, or approximately 40 weeks of gestation. Therefore, for babies born prematurely, the retinal vasculature is both incompletely developed and highly susceptible to pathological maldevelopment. Removal from the physiological environment in utero introduces a multitude of changes, further confounding the otherwise normal developmental progression.
Among the most notable of these environmental changes is blood oxygen levels. Specifically, premature neonates may not acquire adequate oxygen through breathing alone, necessitating oxygen supplementation and sometimes more invasive respiratory support. While these interventions have drastically improved survival rates for premature babies, they also introduce high levels of oxygen that inhibit normal retinal vascular development. This means elevated retinal oxygen will mimic the effects of over-abundant blood vessels, diminishing the expression of the central vascular development regulator, vascular endothelial growth factor (VEGF). As VEGF levels in the retina decline, the retinal vascular development stalls, leaving large avascular zones devoid of blood vessels.
Later, as these neonates receive less invasive respiratory support, oxygen levels in the retina precipitously decline in these avascular zones, leading to a resurgence in VEGF expression. It is at this stage that ROP can progress to blindness as new and highly disorganized blood vessel networks are formed under the influence of VEGF. In these babies, the irregular vascular networks proliferate uncontrollably, a process called neovascularization, which can result in tractional retinal detachment.
As ROP became increasingly well-characterized after the introduction of oxygen supplementation in the 1930s and 1940s, screening for ROP became commonplace and is performed routinely today in premature neonates. When identified at earlier stages, ROP progression can be halted with laser, cryosurgery, or anti-VEGF therapies. However, it is also important to note that these therapies are administered after retinal damage has already occurred and carry the risk of additional ocular damage and poor outcomes.